Cardiac Catheterization Mission: February 2017
Developing a strong rheumatic heart disease (RHD) research infrastructure in Uganda has also resulted in substantial increases in clinical cardiology capacity around the country. A national RHD registry has been created and clinical RHD centers of excellence have been established in three remote referral hospitals. This provided specialized cardiac care for the first time outside the capital. Our collaborative program in Gulu (in Northern Uganda) that grew out of screening research studies has allowed hundreds of patients to receive cardiac care without traveling great distances.
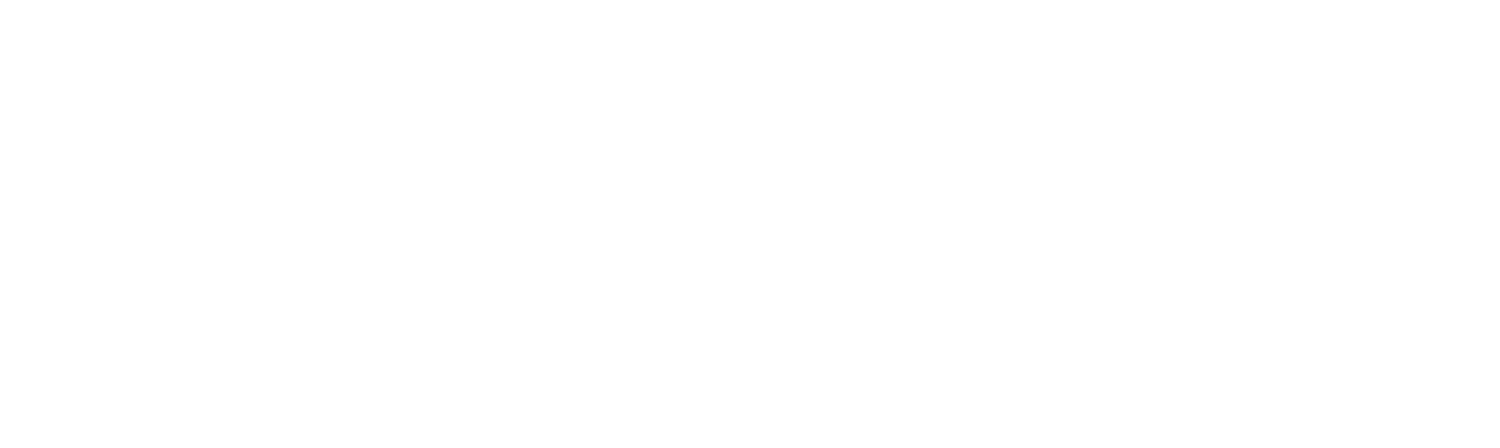
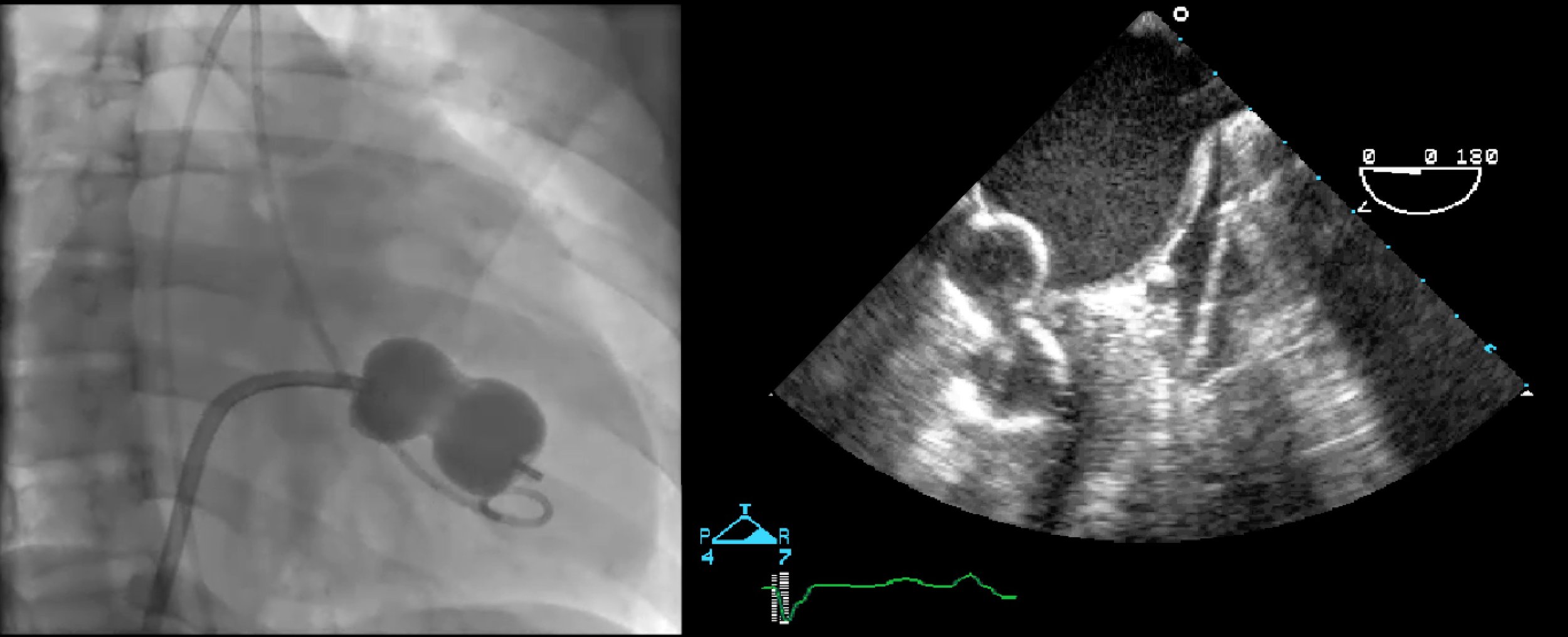
Tertiary services are growing as well, and we have successfully conducted over a dozen training and teaching missions to build a sustainable surgical and cardiac catheterization program, so that children with heart conditions can be cared for at home. Our clinical collaboration has helped foster growth and sustainability at the Uganda Heart Institute. The Ugandan team has performed 13 rheumatic valve surgeries and 40 catheter balloon procedures for rheumatic valve blockage in 2017. The balloon procedure is guided by x-ray and ultrasound as shown here.
Even though Dr. Craig Sable has been working at the Uganda Heart Institute for 15 years, the Heart Healers team had even bigger goals for our February 2017 visit than ever before.
On February 20, we had completed (or at least thought we were done) our first RHD cardiac catheterization mission in Uganda. 10 children and young adults with severe valve blockage had been successfully treated via cardiac catheterization (with a balloon valve dilation procedure, see Figure 2) – all being given a new lease on life without heart surgery. Ugandan cardiologist Emmy Okello had performed all these cases under the supervision of a two-person cardiology team from Brazil, Drs. Maria Nunes and Lucas Lodi. The great success of this mission represented several important new landmarks in our program: treatment of a life threatening disease by a procedure not previously available in Uganda, skill transfer of techniques to Dr. Okello to allow for additional patients to be treated locally, leveraging a “south-south” partnership between our mutual partners in Uganda and Brazil, and the intersection of research and clinical care – several of the patients had been found to have RHD as part of important research projects.
As the final scheduled catheterization was completed, 17-year-old Daniel (shown here) arrived at the Uganda Heart Institute in severe distress. He had come by bus from several hours away and did not have the energy to stand up, he could barely breathe. He underwent an echocardiogram that showed the most severe mitral valve blockage we had ever seen. None of us expected him to survive more than a few hours, but we had to do something. We took him to the cardiac catheterization laboratory and emergently tried to open his valve with a catheter balloon, but the blockage was too severe. His only hope was to go immediately to the operating room for valve replacement. In what was a heroic life saving operation, Ugandan surgeons Tom Mwambu and William Manyilirah replaced one of his valves and fixed another one. Daniel’s first night was very tenuous but 10 days later he walked out of the Uganda Heart Institute and is now active and feeling better than he has felt in years. He will need to be on blood thinning medication for the rest of his life, but our clinical and research collaboration in Uganda helps support making this possible in the Ugandan capital as well as in towns in Northern and Western Uganda.